Do I really need to know my blood glucose if I’m healthy?
.avif)
Sleep trackers, heart rate monitors, calorie counters and pedometers can be seen on people all around the world today, but this is only the beginning.
Wearable electronics are inching closer to the accuracy level of professional medical equipment. Continuous blood sugar monitoring (CGM) systems are the next big thing. Aaron Neinstein, predicts that by 2025 wearable glucose sensors will be as common as other wearables, and not used only by diabetics.
In Silicon Valley, this future has already arrived. More and more entrepreneurs and investors who lead a healthy lifestyle are adding Glucose tracking to their daily routine.
Among these are:
- David Asprey. Bulletproof founder (who has posed for Instagram with a one).
- Mike Brandt and Jeffrey Wu. Founders of brain-boosting startup H.V.M.N., have one.
- Kevin Rose. Digg co-founder.
- Patrick Collison. The CEO of the Stripe electronic payment system.
- Tim Cook. Analysts say that Apple CEO is showing great interest in implementing this technology.
The question of whether or not it will become mainstream remains to be seen, and is dependent on whether the general audience understands the importance of this biomarker.
Why monitor your blood glucose levels if you are healthy?
To begin with, to make sure that you are really healthy. According to the International Diabetes Federation, every second type 2 diabetic is unaware that he is ill. Why is this happening? Because identifying diabetes by the complications it causes is not so easy:
1. The symptoms and complications develop gradually, so that many have time to get used to the new state and begin to perceive it as the norm.
2. The manifestations of hyperglycemia (a chronic increase in blood glucose levels) are very similar to the symptoms of many other disorders which makes it very hard to determine:
- Your head hurts in the morning, you blame it on the coffee or the weather.
- You want to sleep all the time, but at night you suffer from insomnia. You think this is the result of a mundane reason like jet lag, or overwork.
- You often have nightmares, but that’s normal, right?
- You suffer from a frequent urge to urinate: that coffee again.
- You wake up at night with a dry throat: last night’s glass of wine is the culprit, no problem, you put a glass of water on your bedside table.
- You sweat a lot at the slightest physical exertion - you just need to dress lighter.
Edema, bouts of hunger, abrupt weight changes, blurred vision, dizziness, fatigue, depression, frequent colds, intellectual decline, fluctuations in blood pressure, impaired potency in men - all these signs should raise alarm bells for diabetes, but most often they do not.
Who is at risk?
The share of diabetics among the adult population of the planet is growing very rapidly: 4.7% in 1980 and almost doubling to 8.5% by 2014. For almost all of us, this means that the risk zone is expanding. You may be in it if:
- You are over 45 - Mitochondrial disorders increase with age.
- You have close relatives with diabetes - The development of insulin insensitivity has a genetic basis.
- You are overweight - a waist circumference of more than 80 cm for women and more than 94 cm for men is a tell-tale mark of diabetes.
- You have chronic inflammation - certain cytokines released during inflammation can disrupt the insulin signaling system.
- You have hepatitis C - this disease increases the likelihood of developing insulin resistance by 4 times
- Your lipid metabolism is disturbed.
- You suffer from cardiovascular disease.
- You consume too many "fast" carbohydrates (fast food, sweets, pastries).
But doesn’t my doctor test me for that?
Even if you regularly take a biochemical blood test, which includes the level of glucose, and it is normal, this still does not guarantee the absence of diabetes.
A little explanation: immediately after eating, the digestive system breaks down carbohydrates and turns them into glucose. Glucose is then absorbed into the blood from the intestines. When its level in the blood rises, the pancreas produces the hormone insulin. The insulin acts as a key on the cells: it opens them so that they can absorb glucose molecules - their main source of energy.
One and a half to two hours after eating, glucose levels reach a peak, and then begin to decline. One part is absorbed by the cells, the rest is stored in the liver in the form of "animal starch" - glycogen. With periods of fasting, the level of glucose drops, and the pancreas secretes another hormone - glucagon.
It signals to the liver that it is time to break down the stored glycogen and release the missing glucose into the blood. This mechanism helps us maintain energy balance during fasting.
It can also affect the results of the tests - for several reasons:
- After a whole night of fasting, a glass of water in the morning and a trip to the clinic, the glucose level may be lower than usual. Especially if the day before the analysis you had performed physical activity.
- A blood test for sugar is taken "on an empty stomach", that is, approximately 8-12 hours after the last meal. During this period, almost half of the glucose entering the bloodstream is produced by the liver from glycogen. Any alcohol drunk the day before suppresses the process of glycogen breakdown, which means that there will be less glucose in the blood in the morning.
- Some medications taken before bed can also affect your glucose levels. For example, aspirin (reduce) and Valium (increase). See the full list here.
- Infections, stress, and poor sleep cause a temporary decrease in the sensitivity of cells to insulin, as a result, blood glucose levels may be higher than usual.
- Even with diabetes, fasting blood sugar can be lower if you eat a little before bed, which is common with diabetes. In this case, at night, glucose continues to be absorbed into the blood from the intestines, the body does not need to use energy reserves, so the liver does not receive a signal to break down glycogen.
Is there a more reliable analysis?
There is. Glycated hemoglobin (HbA1c) test.
Hemoglobin - the protein component of red blood cells (erythrocytes) - is glycated as a result of the Maillard reaction: the higher the concentration of glucose in the blood, the more actively it combines with hemoglobin and the more glycated hemoglobin in the body. The lifetime of erythrocytes is about 120 days. Therefore, the number of carriers of glycated hemoglobin shows the average blood sugar over the past three months.
The advantage of this indicator is that it does not depend on how much you ate, what you drank, how much you moved, or when you went to bed the night before.
But this is also its drawback: it does not reflect the dynamics of glucose levels. It is impossible to determine exactly when, how often and for what reason there were spikes in blood sugar. This missing piece of information is extremely important.
Why are fluctuations in glucose levels dangerous?
Blood glucose levels can be divided into two types:
- The norm is the reference indicators of a healthy person: 4.0–5.4 mmol/l (72mg/Dl - 97mg/Dl)
- The Safe Range- the lower and upper limits of the safe range of fluctuations in glucose levels after eating and under the influence of various factors: 3.3-7.8 mmol/L (59mg/dL - 140mg/dL)
In the “safe” range, the body is already under stress. Its boundaries are not indicators of health, but threshold values. In fact, they are signals for taking emergency measures: anything above or below these indicators can result in dangerous complications.
If higher than 140mg/Dl:
- Glucose from the blood gets into the urine, which has a devastating effect on the nerves and blood vessels of the kidneys;
- Free radicals are formed: their molecules damage arteries, preventing the body from maintaining stable blood pressure and increasing the risk of stroke;
- The risk of developing cancer increases due to the high concentration of the growth hormone insulin in the blood: due to its enhanced production, the pancreas tries to cope with excess glucose.
If lower than 59mg/Dl, a person can experience :
- Bouts of dizziness
- Convulsions
- Hallucinations
- Stroke
- Cerebral edema and coma
Are there sugar spikes in healthy people?
Yes. In 2018, Stanford University conducted a study of 57 people, most of whom were diagnosed as healthy on standard tests. For 2–4 weeks, they underwent 24-hour glucose monitoring. It turned out:
With a general moderate background, jumps in sugar levels in some healthy people can reach a diabetic level - up to 11 mmol/L (198mg/dL - higher than the safe limit)
In accordance with the variability of glucose levels (weak, moderate and strong), the researchers divided the subjects into three glucotypes. As the frequency and amplitude of fluctuations increases, so does the average glucose levels in each group: 4.2 - 5.3 - 6.7 mmol / l.
Moreover, despite the fact that, on average, the indicators for the first two glucotypes are quite normal, at the time of the jump they can exceed not only the norm, but also the permissible limit.
What is your glucotype? Without round-the-clock monitoring, this is simply unknowable, as well as two other important parameters:
1. Individual glycemic response to foods. When choosing foods, you can, of course, be guided by their glycemic index: a measure of the level to which blood sugar rises after eating them. For the standard (100 units), it adopted the effect of pure glucose. But studies have shown that in fact, the glycemic impact of the same product varies greatly depending on the characteristics of the organism. In other words:
Strawberry shortcake can affect you very differently than it does others
2. Relationship of glucose levels with other conditions. When he was hosted in the Joe Rogan podcast, renowned gerontologist David Sinclair told Roganhow his biologist colleague Rhonda Patrick discovered, through 24-hour glucose monitoring, that the main cause of her sugar spikes was not the much despised potato (GI 95), but actually, the healthier grapes (GI 45)
We know from research what changes an increase or decrease in glucose levels can cause. For example:
In people with high blood sugar, the brain ages 9 years faster. But without constant monitoring, it is impossible to understand whether specific cases of intellectual decline or sleep disturbance are due to blood sugar, and not other factors
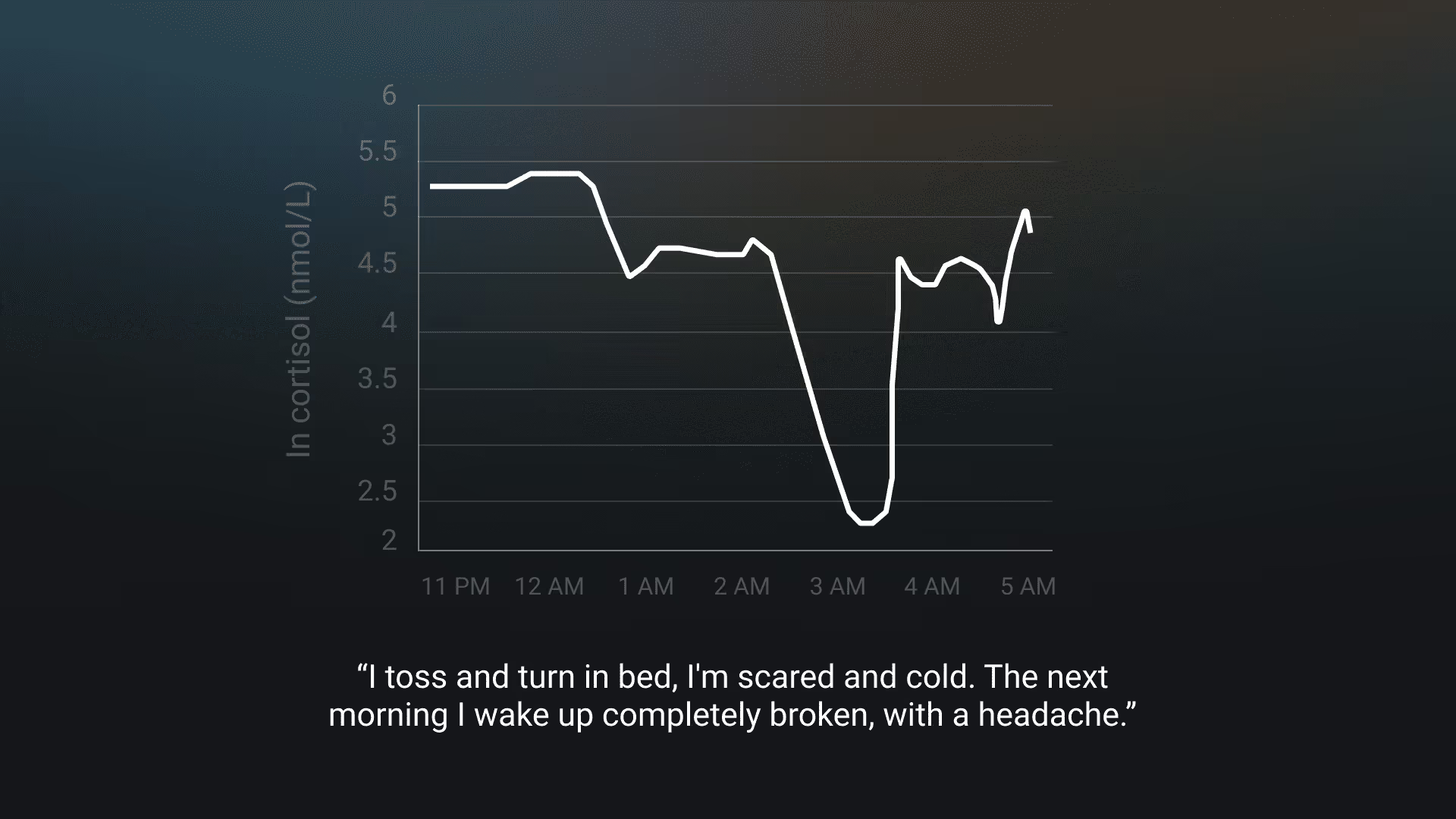
A simple example: biohacker Justin Lawler conducted a test on synchronous monitoring of sleep and glucose. And found a sharp drop in sugar levels (up to 3 mmol / l), which correlated with poor sleep and morning headaches. At the same time, the morning indicators were normal. If he had limited himself to them, the connection would have remained unnoticed.
How to test?
A regular glucometer with a needle and test strips is not an option. It can't take readings all the time unless you agree to pierce your finger every half hour. But in this case, be prepared to give up the keyboard and switch to voice control of the computer.
There are some really promising non-invasive and minimally invasive glucose measurement technologies. One of NovioSense's most interesting startups is a mini-sensor for continuous monitoring that is placed under the lower eyelid of the eye and can capture the smallest fluctuations in tear fluid glucose levels.
FreeStyle Libre

The heart of the system is a white plastic disk-shaped sensor a little larger than a five-ruble coin. On the one hand, it has a thin thread (less than 0.4 mm thick), which is painlessly inserted under the skin to a depth of 5 mm and measures the level of glucose in the interstitial fluid. On the other hand, there is a storage device that automatically saves readings every 15 minutes and transmits data via a built-in bluetooth transmitter to a special reader or smartphone with a proprietary application. With the sensor, you can take a shower and even swim. The libre is completely FDA approved.
- Lifetime of one sensor: 14 days
- Disadvantages: You will have to periodically bring the reader or smartphone to the sensor in order to read the indicators (this can also be done through clothing).
- One sensor lasts for: 14 days.
- Price: $137.63 per 2 sensors
Dexcom

It is similar in design and operation to the FreeStyle Libre, but the sensor is capable of transmitting data to a smartphone or Apple Watch on its own. The sensor and transmitter can withstand showering and swimming in the pool. The device takes readings 288 times a day (day and night) with a frequency of 5 minutes. Able to draw a continuous graph of changes in glucose levels and warn in case of sharp fluctuations or reaching the set values. FDA approved.
- One sensor lasts for: 10 days.
- Price: A set of three sensors - $349. Two bluetooth transmitters for sensors - $475. Scanner - $365.
Eversense

Unlike the previous two devices, the sensor is implanted under the skin. The sensor's fluorescent chemical coating generates light when it comes into contact with glucose in the tissue fluid. The light signal is converted into digital readings, which are transmitted every 5 minutes by a bluetooth transmitter to a compatible mobile device. The Eversense mobile app can also alert you when your glucose levels are too low or too high. You can also set it to individual values. In addition, measurements can be programmed for a specific time: meals, workouts, etc. FDA approved
- Lifetime of one sensor: 90 days.
- Disadvantages: The system must be calibrated at least twice a day by comparing the sensor data with the glucometer readings.
- Price: $ 99 plus the cost of installing the implant.
Summary
According to the results of clinical trials, all three devices are quite accurate. The Mean Absolute Relative Deviation (MAD) compared to laboratory data is less than 9% for Eversense, less than 10% for Dexcom, and 9.4% for FreeStyle Libre. But life is harder than tests. If the sensor readings suddenly start to go off scale, do not rush to panic.
Gerontologist David Sinclair had an oddity with the FreeStyle Libre sensor: once, judging by the readings of the device, he himself did not notice how he survived a diabetic coma. The cause of the miracle was an accidental impact on the sensor during training.
About us
With the help of a Freestyle Libre Continuous Glucose Monitor and a coach, you can achieve the wellness goals you set for yourself. With the Aspect 21-Day Checkup Plan, you will receive constant guidance as you learn how your body processes sugar and how it affects your mind and your body. Research shows a distinct causal relationship between Glucose and Stress, Sleep Quality, Physical Fitness, and even Adhd, PCOS, and Conception. With the aspect plan you will be able to test your body’s reactions to a set of personalized experiments and improve your overall well-being.
Try the Aspect 21 Day Checkup today!






.avif)

.avif)
